Zenker’s Diverticulum
By Reid Wasserman, DO, Klaus Mönkemüller, MD, PhD, Adil S. Mir, MD FACP
Virginia Tech Carilion School of Medicine, Roanoke, Virginia, USA
Department of Internal Medicine, Division of Gastroenterology

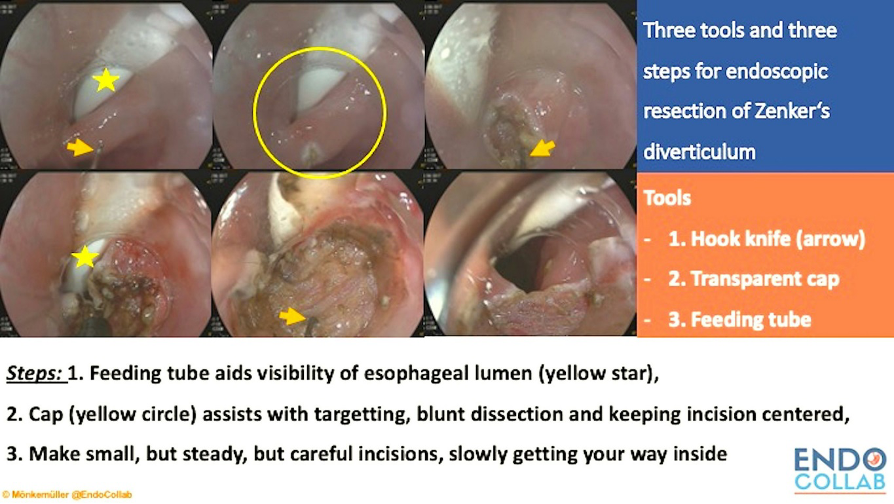
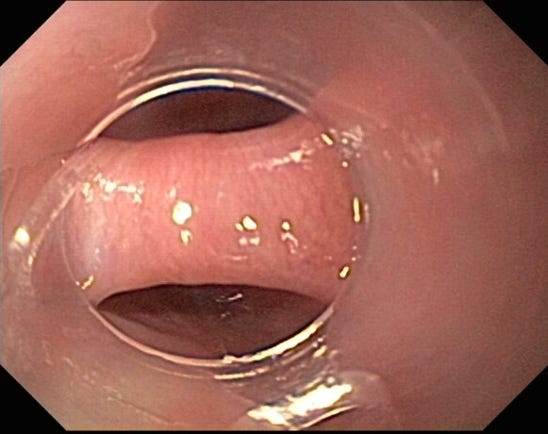
An elderly male presented with dysphagia to solid food, halitosis, and regurgitation. The patient also lost about 10-kg over a 6-month period. Subsequently, the patient underwent an EGD. Note the slit-like entrance to the esophagus. On the next image, a feeding tube is seen in the esophageal lumen. A thin feeding tube is advantageous when endoscopically resecting a Zenker diverticulum for the following reasons:
(a) the tube serves as a reference point to differentiate the esophageal lumen from the diverticulum, (b) It helps guide the incision exactly in the middle of the Zenker's bridge, (c) placing a feeding tube creates a conducible environment for healing and allows for enteral nutrition.
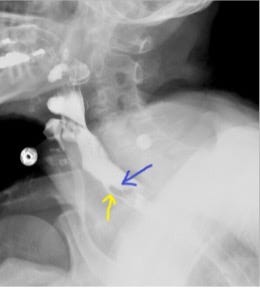
Depicted below are the barium swallow images. The Zenker’s diverticulum is identified by the posterior location (blue arrow). The contrast barely enters the esophagus (there is a functional stenosis) (yellow arrow).

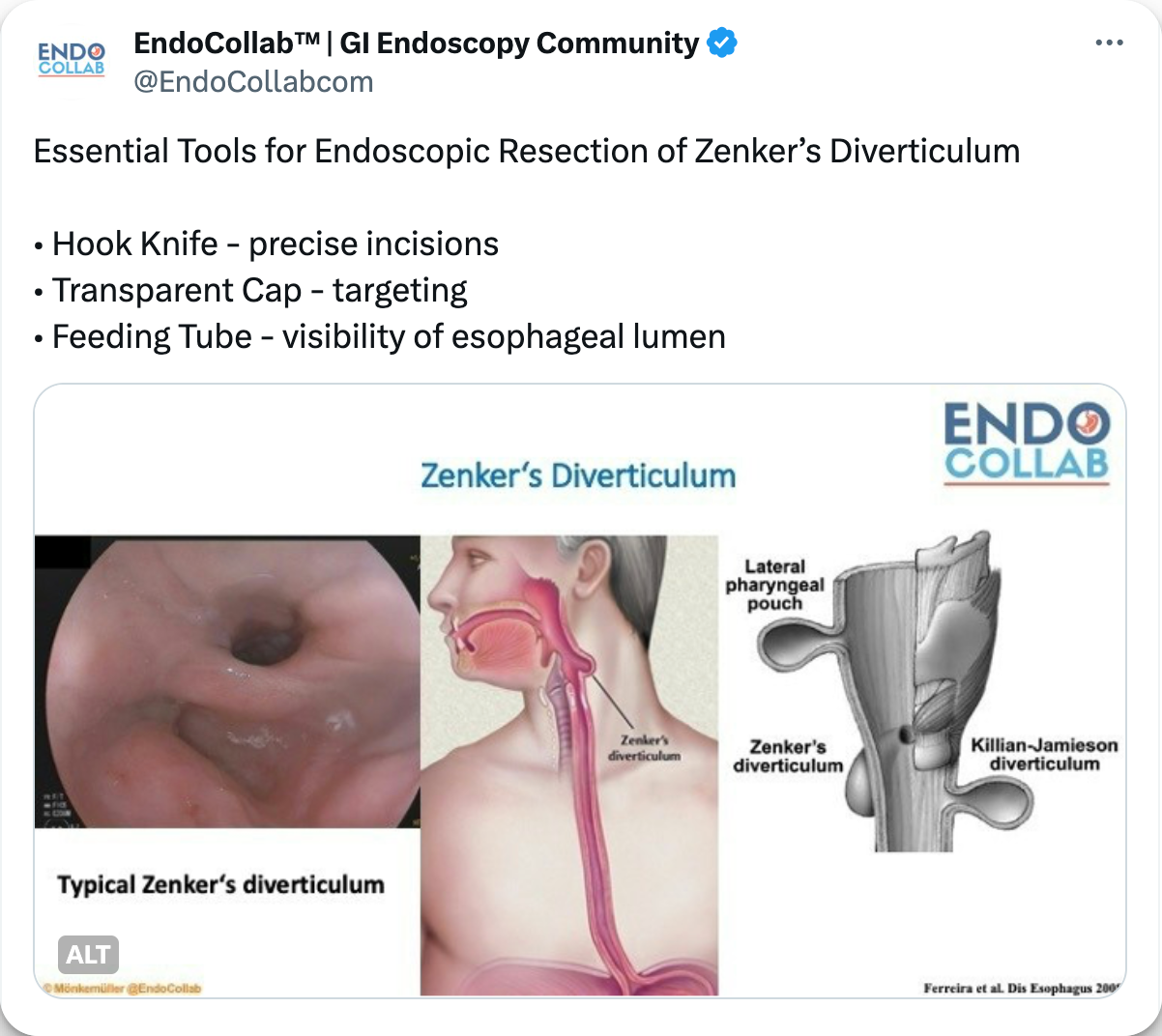
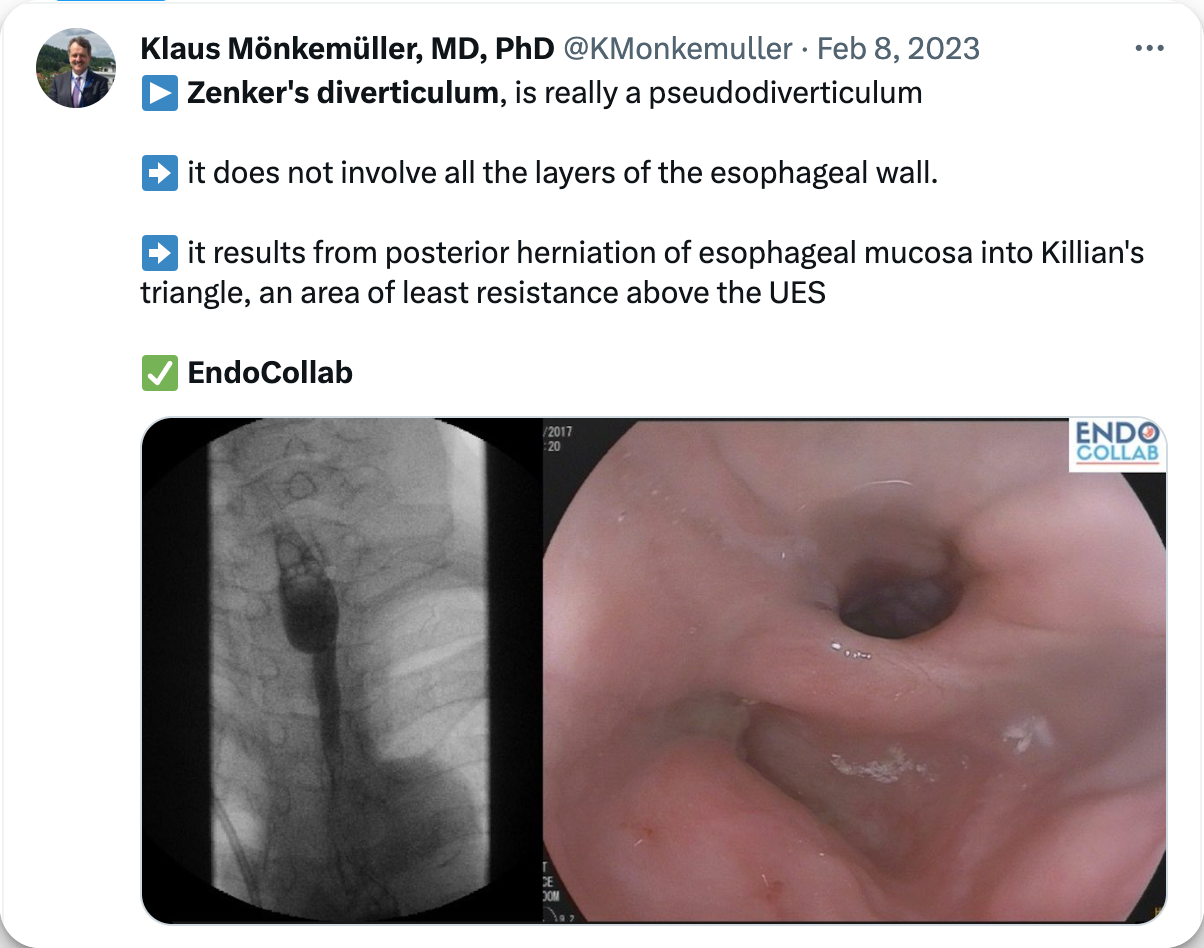
Zenker's diverticulum, also known as a posterior pharyngeal pouch, is really a pseudodiverticulum, as it only contains mucosa and submucosa. This pseudodiverticulum results from posterior herniation of esophageal mucosa and submucosa into Killian's triangle, an area of low resistance situated above the upper esophageal sphincter (cricopharyngeal muscle) and below the inferior pharyngeal constrictor muscle.
Zenker’s diverticulum typically presents in adults by the sixth or seventh decade. Clinical presentation includes: dysphagia, the pooling of food within the diverticulum, which can cause bad breath, and frequent regurgitation. Serious complications include aspiration and malnutrition (1), which may lead to chronic cough or pneumonia. The gold standard tool for diagnosis is barium swallow and continuous fluoroscopy (2). If there is high clinical suspicion for Zenker’s diverticulum, one may choose to obtain a barium swallow before proceeding directly to endoscopy as it is possible to navigate into the diverticulum and cause potential perforation.
The most common treatments are open surgical diverticulectomy with or without cricopharyngeal myotomy, or rigid and flexible myotomy (1). The myotomy consists of an incision at the “neck” of the diverticulum, from the mucosa, then through the submucosa, and finally the muscle (“myotomy”).
The use of a distal transparent endoscopic cap may assist during the incision/resection process.
In this case of Zenker's diverticulum we can see how the cap:
(a) stabilizes the view
(b) allows for focused attention of the target
(c) maintains a safe distance between the scope tip and the diverticular septum. All of these aspects permits a directed and controlled incision. Additionally, the cap allows for blunt dissection and the ability to achieve hemostasis via tamponade if any bleeding were to occur.
Don't miss the quick tip video on Zenker's resection.
Although open surgical techniques have historically been the gold standard for treatment, endoscopic options have become more popular (3). Cricopharyngeal myotomy using flexible endoscopy is a safe and effective technique for the management of Zenker's diverticulum. Potential benefits of this approach include shorter operative times, shorter postoperative admissions, and earlier progression of diet (3).
References:
Ferreira LE, Simmons DT, Baron TH. Zenker's diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21(1):1-8.
Pescarus R., Shlomovitz E., Sharata A.M. Trans-oral cricomyotomy using a flexible endoscope: technique and clinical outcomes. Surg Endos. 2016;30:1784–1789.
Fan HS, Stavert B, Chan DL, Talbot ML. Management of Zenker's diverticulum using flexible endoscopy. VideoGIE. 2019 Jan 30;4(2):87-90. doi: 10.1016/j.vgie.2018.12.007. PMID: 30766952
EndoCollab. EndoCollab is an online community for GI endoscopists. With 1200+ members, endoscopists discuss interesting cases, view on-demand video courses, and get new endoscopy tips every day. Join EndoCollab